
Patient receives a COVID-19 vaccine and health workers help ensure his paperwork is complete at Patan Hospital in Nepal.
Beyond the Triple A: building resilience in health systems through agility
2 May 2024
Hema Bhatt [opens new tab], of OPM Nepal, has recently been involved in a technical assistance programme in the country which seeks to strengthen sub-national health systems through support to public financial management (PFM). In this blog post she explores the importance of agility in Nepal’s COVID-19 response.
The healthcare landscape in Nepal is a dynamic and complex system, constantly evolving in response to emerging challenges. This demands the ability to implement policy changes and also the authority to make necessary adjustments and secure stakeholder buy-in. In today’s volatile, uncertain, complex, and ambiguous (VUCA) world, agility has emerged as a crucial element for navigating the dynamic “change space” where multifaceted challenges are addressed. While frameworks like the Triple A (Ability, Authority, Acceptance), employed by the Problem Driven Iterative Adaptation approach, emphasize many core competencies for navigating change, they often overlook agility.
The Triple A Framework highlights three key aspects:
• Authority: Legitimate power to make and enforce decisions.
• Ability: Capacity to execute initiatives, including the necessary skills, resources, and infrastructure.
• Acceptance: Stakeholder willingness to support and comply with proposed changes.
This blog post delves into Nepal’s response to the COVID-19 pandemic, using a PFM lens to illustrate the importance of agility within the Triple A Framework. It will demonstrate how Nepal successfully adapted its PFM system while upholding accountability and transparency.
The Triple A Framework in action: Nepal’s response to COVID-19
Nepal’s Ministry of Health and Population (MoHP) effectively led the COVID-19 response, demonstrating all three elements of the Triple A Framework:
• Authority: The MoHP’s position as the apex health body granted them the legitimate power to develop and enforce essential policies, manage external relations, coordinate efforts across sectors and use their service delivery network.
• Ability: The MoHP rapidly skilled up its workforce, identified additional domestic and external resources and fostered collaboration with stakeholders to adapt to the unique challenges of the pandemic.
• Acceptance: Facing the urgency of the situation, stakeholders readily accepted the MoHP’s leadership and necessary changes, minimizing delays in implementing crucial measures.
However, the rapidly evolving nature of the pandemic demanded an additional element: agility.
Agility: The crucial element in navigating crisis
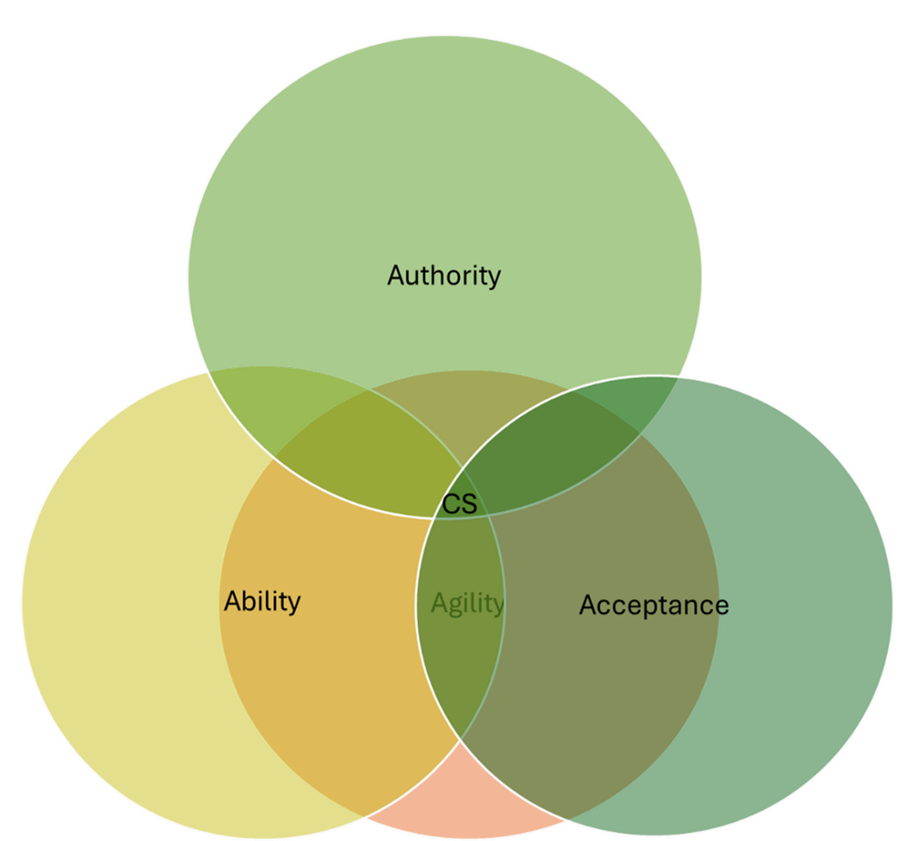
Figure 1: Change space (CS) navigation as an interaction between authority, ability, acceptance, and agility.
While the Triple A Framework provides a solid foundation, agility is equally important for navigating the “change space.” Agility refers to the ability to adapt quickly and make efficient decisions in response to changing circumstances, crucial during unforeseen challenges like COVID-19.
Nepal’s PFM system adaptations during COVID-19 exemplify agility in action:
• Flexible budgeting: The pandemic exposed the inflexibility of existing PFM procedures. A special decree enabled swift reallocation of funds within the health sector, prioritizing COVID-19 needs. Rapid epidemiological modeling further informed resource allocation decisions.
• Streamlined external support: A “one-door” policy streamlined external support, minimizing duplication, and enhancing efficiency, transparency, and accountability.
• Adapting procurement: The urgency of the situation necessitated deviations from standard procurement procedures. Decentralized procurement for COVID-19 supplies, while necessary, presented coordination challenges. To address this, a separate COVID-19 budget line item was created for easier tracking. Additionally, a decree allowed for flexible emergency procurement with adequate controls. Standard operating procedures and technical specifications were updated to streamline procurement across all levels, improving efficiency and transparency. Digitization of these specifications further facilitated access during mobility restrictions.
• Service costing and guidelines: The costing of the direct cost of COVID-19 treatment guided resource allocation decisions. Comprehensive financial guidelines were developed for service procurement from both public and private sectors, implemented in partnership with MoHP. These guidelines enhanced transparency and accountability, optimizing resource use.
• Oversight and monitoring: In 2022, the Office of the Auditor General conducted a comprehensive COVID-19 audit across all government levels (federal, provincial, and local) and sectors (finance, health, defense, home affairs and urban development) involved in pandemic management. This special audit aimed to enhance oversight and ensure transparency in how COVID-19 funds were utilized. The report offers valuable insights and lessons learned, providing a crucial resource for future efforts in controlling and mitigating similar pandemics from a financial management perspective.
Balancing agility with accountability in PFM systems
While PFM systems prioritize uniformity and accountability, introducing agility requires careful consideration of risks and safeguards. Nepal’s agile adaptations facilitated resource mobilization, procurement, and service provision, but challenges emerged. Transfers of funds to the provincial and local levels were sometimes delayed, fragmented and less than anticipated. Limited data on COVID-19 funds received and spent hindered optimal resource use and monitoring. Existing PFM weaknesses, such as poor internal controls and limited oversight capacity at the sub-national level, also created vulnerabilities, as evidenced by concerns about false documentation in private sector claims.
The COVID-19 pandemic highlighted the importance of building a resilient PFM system that can adapt while upholding core principles of accountability and transparency. This necessitates:
• Investing in sub-national PFM systems: Strengthening internal controls and oversight capacity is crucial for effective resource management, especially in agile decision-making contexts.
• Nuanced adaptations: Changes to PFM processes should be carefully designed with clear safeguards to mitigate risks and ensure accountability. Rigorous monitoring and evaluation are vital to assess the effectiveness of adaptations.
• Continuous learning and improvement: Fostering a continuous cycle of learning through action, reflection, adaptation, and further action allows for real-time adjustments in response to evolving challenges.
Nepal’s COVID-19 response demonstrates that agility, alongside the Triple A Framework, is essential for navigating complex challenges in healthcare systems. Recognizing the need for a balance between agility and accountability, continuous learning, and strengthening sub-national systems is crucial for building long-term resilience in a VUCA world.
Further information
This blog post derives from a study Strengthening subnational health systems through support to public procurement and financial management: lessons from a technical assistance programme in Nepal. More on that work here.
Image: Nepal Patient Receiving Vaccine. USAid via Flickr [opens new tab] CC BY-NC 2.0 DEED. Attribution-Non Commercial 2.0 Generic