What could global health initiatives look like?
29 August 2023
The Future of Global Health Initiatives (FGHI) process has recently delivered the Wellcome-commissioned report, ‘Reimagining the Future of Global Health Initiatives’ (read it here – opens new tab). Featuring contributions from ReBUILD partners, Queen Margaret University (QMU), the report draws on several data sources, including the perspectives of more than 300 experts at global, regional, and country levels, and proposes a vision for how global health initiatives (GHIs) could be optimised to support countries’ progress towards universal health coverage (UHC). A recent webinar presented the findings of the report and is summarised here.
What is the FGHI?
The session was introduced by Dr Mercy Mwangangi, FGHI Co-Chair and Chief Administrative Secretary, Ministry of Health, Kenya. She explained that over recent decades GHIs have contributed to enormous progress in protecting lives, improving the health of people globally, and delivering on the Millennium Development Goals (MDGs). There is, however, increasing recognition of the need for greater attention to overarching, system-level coordination and structure of GHIs and their interface with other actors to better align investment behind Agenda 2030 and Sustainable Development Goal 3, hence the FGHI process.
Dr Mwangangi explained that the FGHI process is a time-bound multi-stakeholder process of dialogue, research, deliberation and action. It seeks to identify and enable options for global health initiatives to better complement domestic financing to maximize country-level health impacts, as part of country-led trajectories toward UHC. The process also considers the roles, responsibilities, and ways of working of other global health actors and their interface with GHIs, to foster better alignment and coherence of all external health finance and technical assistance to countries.
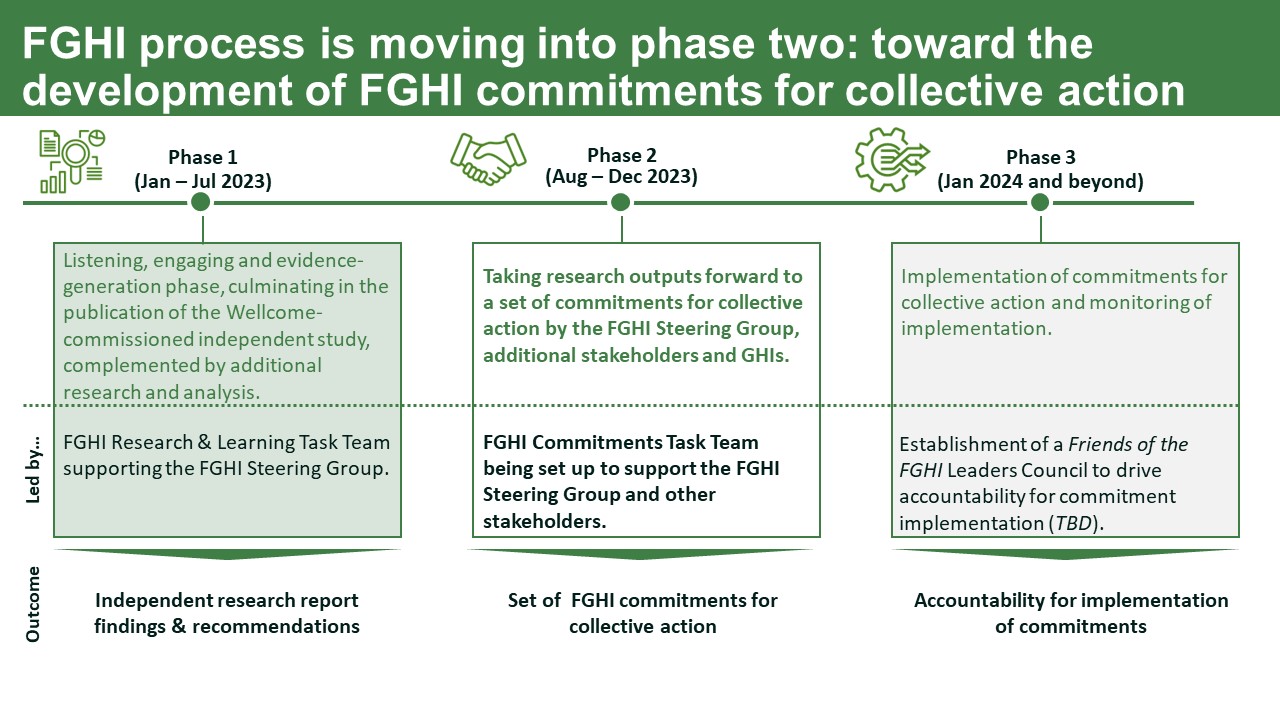
January to July was essentially the ‘listening phase’ – the first phase. The process has now entered its second phase (see the below image for details of all three phases) which involves taking research outputs forward to form a set of commitments for collective action by the FGHI Steering Group, stakeholders and GHIs.
What does the report seek to achieve?
Professor Sophie Witter of QMU and ReBUILD for Resilience then introduced the report and described its findings and recommendations. The report is a key independent input to the FGHI process, complemented by analyses and case studies from other bodies including WHO, Institute for Health Metrics and Evaluation, World Bank, OECD, SDG 3 GAP, Lancet Commissions and the UK’s Foreign, Commonwealth and Development Office.
Professor Witter outlined the report’s three basic aims:
• To outline a vision of what the GHIs should seek to achieve over the next 15-20 years to strengthen health system capacities and deliver health impacts
• To analyse the extent to which GHIs’ current mandates and ways of working will need to evolve to enable them to effectively, efficiently and equitably deliver this vision, and the contextual factors that would support or hinder such a shift
• Finally, it provides recommendations on how and when the GHIs’ current mandates and ways of working should evolve
Six focal GHIs were selected for study by FGHI. Key informants came from 66 countries. They provided a wide range of views (some very radical) but most falling within the ‘critical friend’ perspective.
The landscape and GHIs today
There was the recognition that many countries are not on track to achieve UHC by 2030. Substantial achievements were made in many indicators in the MDG era (up to 2015), but the situation has been plateauing since. Financial protection has generally not been improving or has worsened in most regions. There has been an increase in the number and diversity of actors in global health. Four ‘mega-trends’ have been witnessed – proliferation (more GHIs), verticalization (focusing on specific areas), circumvention of government systems, and fragmentation (a lack of coordination among actors). Also, there’s a lack a funding to reach SGDs.
The focal GHIs are very diverse but have six main roles: market shaping, R&D of new technologies and medicines, grant giving, provisional of technical assistance, purchase and supply of commodities, and advocacy.
Looking ahead, the landscape offers a range of quite daunting challenges for countries including growing and emerging health threats, a stormy geopolitical climate, and a likely growth in migration and refugees, leading to more problems that need to be tackled at regional level (not just national). The growth in new technologies will help states to respond to those challenges but will also create cost burdens and choices.
The GHIs studied exhibited a range of some quite significant strengths and contributions, but also some concerning weaknesses which Professor Witter went into. Several demonstrated innovative financing for global health, pooled procurement, ensuring access to vaccines, a willingness to reach excluded groups, adaptability and some progress on alignment. However, they also exhibited a lack of credibility in the use of metrics to measure outcomes and contributions, a lack of transparency in funding and impact, in-country models with complexity and accountability up but not down, and limited fundraising from the private sector.
All GHIs studied are invested in political economy dynamics, with the GHIs solving many funders’ problems by creating structures which converted funding into credible results. At the national level, clients were created who gained resources and therefore power from the funding. However, power was not evenly dispersed, and was perceived as focused in some key actors, including funders.
Looking to the future for GHIs
The team has proposed a vision for future roles of GHIs:
“A global health system where all actors, including GHIs, contribute effectively to the achievement of country-led UHC and hence equitable population health and wellbeing.
This means that all actors, including GHIs, plan, fund, evaluate and account for their funds and programmes to national governments in a coherent and integrated way, working in synergy with other global health actors and based on their comparative advantage, countries’ priorities and needs, and the imperative to build country capacity to sustain UHC (including PHC) through strong and resilient health systems.”
The group has also made six key areas of recommendations for the GHI environment, underpinned by a series of vital foundations including being responsive to countries’ needs, being adaptive and dynamic, and supporting equitable UHC delivery:
1. Make a stronger contribution to UHC, including emerging disease burdens.
2. Strengthen, or at least do no harm, to health systems.
3. Reduce costs for countries and increase efficiency and effectiveness of GHI investments.
4. Support country ownership, capacity building, and chart a clear path to end dependence on GHIs.
5. Enforce more effective alignment between GHIs and wider actors.
6. Limit proliferation of GHIs, and instead focus on strengthening existing architecture.
That change will, of course, need to be carefully managed, requiring action by governments, funder alignment, and a cross-GHI mechanism for following-up the recommendations. Whether there is a window for change is not clear, but the shifting context and shortage of progress to UHC requires improvement. The report found that GHIs have a responsibility to support governments’ efforts to strengthen health systems and achieve UHC by ensuring their investments are coherent with sustainable system strengthening, and do not undermine or distort national investment priorities, including in emerging priorities.
What next?
John-Arne Røttingen, Ambassador for Global Health, Ministry of Foreign Affairs, Norway then took over the presentation, describing how the report fits into the overall FGHI roadmap. It is hoped that the independent recommendations will inform the next phase of the FGHI process and ensure that crucial discussions about the future of the global health ecosystem are grounded in the experience and perspectives of key stakeholders and lessons learned from previous alignment and coordination initiatives. There is a feeling that political commitment to the FGHI process is growing. For example, the process is fully aligned with Africa CDC’s New Public Health Order and the Africa Health Leaders’ Policy Forum is expected to issue an FGHI position statement at its imminent meeting. There is cause for optimism.
There’s further information on the whole FGHI process, as well as the report itself, on the FGHI website [opens new tab]. The report will shortly be available in other languages.